Optic Neuritis
Optic neuritis is inflammation of the optic nerve, often linked to multiple sclerosis (MS). It can also occur in people with infections or immune conditions such as lupus.
Symptoms
- Eye pain or discomfort, especially with eye movement
- Loss of color perception
- Loss of visual field
- Vision loss in one or both eyes
Tests & Diagnosis
Blood Tests: Detect conditions associated with optic nerve inflammation, such as NMO IgG or anti-MOG IgG.
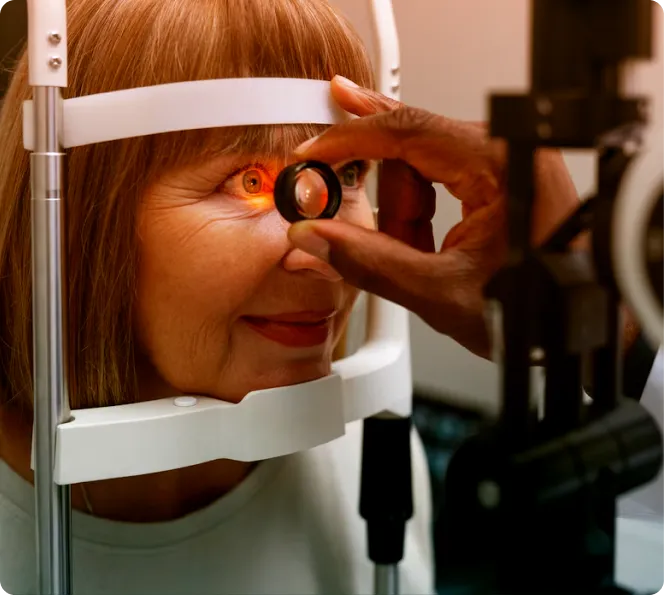
Comprehensive Eye Exam: A detailed evaluation of eye health and overall medical history.
Ophthalmoscopy: A bright light is used to examine the optic disk, which may appear swollen in about one-third of cases.
Optic Nerve Photography: Documents the degree of swelling in the optic nerve.
Visual Field Test: Assesses both central and peripheral vision.
Treatments
Steroid Medications: Often administered intravenously, steroids reduce inflammation and help restore vision.
Why Choose Bascom Palmer Eye Institute?
Ranked #1 by U.S. News & World Report
- The top-rated facility in the country for eye care.
Comprehensive, Multi-Specialty Care
- Our team provides seamless access to experts across medical specialties, ensuring coordinated care for eye conditions linked to broader health issues.
Patient-Centered Excellence
- Receive advanced treatments in a compassionate and supportive environment.
FAQ
What is optic neuritis, and why does it often feel like a sudden eye crisis?
Optic neuritis is inflammation of the optic nerve, the high-speed cable beaming visual info from eye to brain, often kicking off with sharp pain when moving the eye and rapid vision drop—like a short circuit dimming your inner screen. It’s commonly the first hint of multiple sclerosis (MS) in young adults, triggered by immune attacks on the nerve’s myelin sheath, but can also stem from infections or vaccines. Affecting one eye usually, it peaks in days but rebounds mostly, though color vision might stay washed out.
Who is most likely to experience optic neuritis?
It strikes hardest in women aged 20-40, with MS links in 50%—genetics, low vitamin D, or northern latitudes up the odds. Viral prodromes (like a cold before) or autoimmune flares (lupus) add risks, while kids get it post-mycoplasma. It’s not contagious, but if you’ve had one episode, chats with neurologists about MS screening become routine to stay ahead.
How do doctors diagnose optic neuritis effectively?
A relative afferent pupillary defect test (swinging flashlight shows sluggish response) plus visual field charts revealing central blind spots clinch it, alongside MRI brain scans hunting white matter lesions that scream MS. Blood work rules out Lyme or sarcoid, and VEP measures nerve conduction delays—it’s a swift, mostly painless puzzle, often diagnosed in one visit to kickstart recovery.
What are the best treatments to speed up optic neuritis recovery?
High-dose IV corticosteroids (like methylprednisolone for 3-5 days) hasten vision return by days, not weeks, though they don’t alter long-term outcomes. Plasma exchange helps steroid-resistant cases, and for MS ties, disease-modifying therapies (like ocrelizumab) prevent relapses. Pain eases with NSAIDs; most regain near-normal sight in 4-6 weeks, but low-vision rehab polishes any residuals.
What can people do to manage optic neuritis and reduce recurrence?
Sun protection cuts UV-triggered flares, vitamin D supplements bolster immunity, and stress management (yoga, anyone?) dials down autoimmune heat. If MS looms, early meds slash attack risks by 50%; annual neuro-ophtho teams track subtle changes. Survivors often share: “”It was scary, but emerging stronger””—with tools like prism glasses for lingering blur, life refocuses clearly.
Our Doctors
No doctors available for this speciality.
Questions? We’re here to help.
Our appointment specialists are ready to help you find what you need. Contact us today.
