Pediatric Myopia (Nearsightedness)
Myopia is the medical term for nearsightedness, one of the most common eye conditions in children and adults. Children with myopia can see close objects clearly, but objects farther away appear blurred. This happens when the eye grows longer than normal from front to back or when the cornea is too steeply curved, preventing light from focusing correctly on the retina.
In recent years, myopia has been on the rise among children. Research shows:
- 1 in 4 parents has a child with myopia.
- 75% of children with myopia are diagnosed between ages 3 and 12.
- Worldwide, nearly 50% of all people have some degree of myopia.

What Causes Myopia?
Experts are still studying why childhood myopia is becoming more common. The American Academy of Pediatrics suggests that lifestyle factors—such as spending more time indoors, using tablets and phones, playing video games, and doing other close-up tasks—may play a role. Limited time spent outdoors is also believed to contribute.
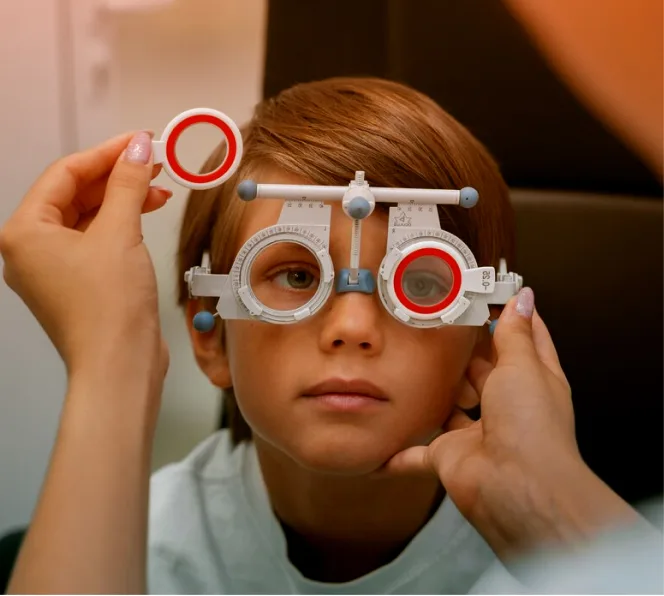
How is Myopia Diagnosed?
Many parents assume that vision screenings at school or at the pediatrician’s office are enough—but they are not. In fact:
- Routine school screenings miss up to 75% of children with vision problems.
- Only 4% of the necessary eye tests are included in standard school screenings.
The best way to detect myopia early is through comprehensive, in-person eye exams. Children with a family history of myopia should be examined as early as 13 to 18 months of age. Early detection is key to preventing progression.
Treatments to Clear Vision
Traditional myopia treatments improve vision but do not stop progression. These include:
- Glasses: The most common treatment. Your child may need to wear them full time or part time, depending on severity. Options include sports goggles and specialized fits for comfort and activity.
- Contact Lenses: Suitable for older children, providing clear vision without glasses.
Treatments to Manage Myopia
Because single-vision glasses and contacts do not slow progression, children remain at risk of developing serious eye conditions later in life. New treatments focus on slowing myopia progression:
- Low-Dose Atropine Eye Drops: Taken nightly, these drops slow eye growth and prevent worsening myopia.
- Myopia Management Contact Lenses: Worn daily and safely discarded at night. These lenses provide clear vision while slowing myopia progression using peripheral defocus technology.
- Orthokeratology (Ortho-K): Specialty lenses worn overnight to reshape the cornea temporarily, improving distance vision and slowing myopia progression.
- Lifestyle Adjustments: Encouraging more outdoor play and limiting screen time can help reduce risk and slow progression.
Early treatment = lower myopia, better quality of life, and reduced risk of vision-threatening eye diseases later in life.
Why Choose Bascom Palmer Eye Institute?
#1 in the Nation
- Ranked America’s No. 1 eye hospital by U.S. News & World Report.
Patient-Centered Care
- We understand how vision affects every part of a child’s life. Our team provides compassionate, effective care with fast and accurate diagnosis.
University-Based Medicine
- As part of the University of Miami, we provide access to state-of-the-art technology, advanced treatments, and clinical research trials.
Skilled Pediatric Specialists
- Our pediatric ophthalmologists and optometrists use child-focused techniques to make exams and treatments comfortable for children of all ages.
FAQ
What is pediatric myopia, and why is it surging in kids today?
How do parents spot and assess myopia in their children?
What proven strategies slow down pediatric myopia progression?
Are there risks if pediatric myopia isn't managed early?
How can families incorporate myopia control into daily routines?
Our Doctors
No doctors available for this speciality.
Questions? We’re here to help.
Our appointment specialists are ready to help you find what you need. Contact us today.
