Toxic Optic Neuropathy

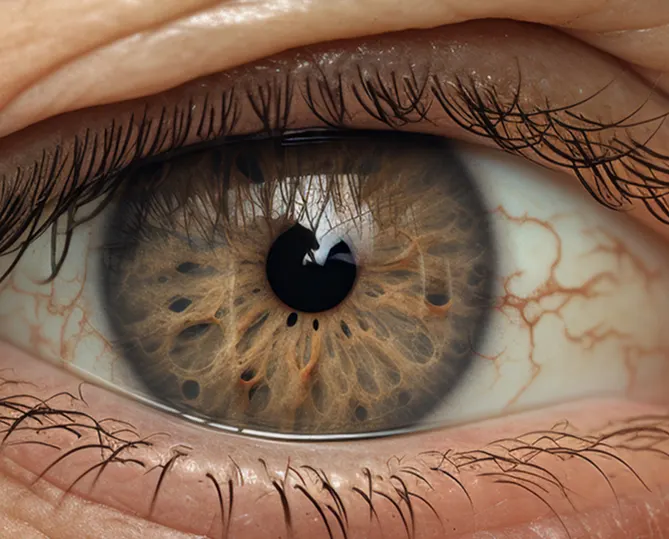
Pupillary abnormalities occur when there is a problem with your pupils – the black center of the eye that controls how much light enters. These conditions can affect vision, eye movement, and eye comfort.
Common Types of Pupillary Abnormalities
Anisocoria: Unequal pupil sizes.
Horner’s Syndrome: Disruption of the nerve pathway from the brain to one side of the face and eye.
Third Nerve Palsy: One eyelid may droop completely, and the affected eye may turn outward and downward.
Adie’s Tonic Pupil: One pupil is permanently dilated and unresponsive to light and other stimuli.
Symptoms
Signs that may indicate a pupillary abnormality include:
- Unequal pupil size
- Difficulty focusing on near objects
- Double vision (diplopia)
- Drooping eyelids (ptosis)
- Eye pain
- Headache or fever
- Sensitivity to light (photophobia)
- Limited eye movement
- Reduced sweating on one side of the face
Tests
To confirm a diagnosis of myasthenia gravis, your doctor may recommend:
Comprehensive Eye Exam
Your ophthalmologist will examine your eyes and review your medical history. Tools like an ophthalmoscope may be used to check the optic nerve and retina.
Imaging
MRI or CT scans may be ordered to determine the underlying cause. Ultrasound of the eye can help distinguish pupillary abnormalities from other optic nerve disorders.
Lumbar Puncture
In certain cases, a spinal tap may be used to measure cerebrospinal fluid pressure and check for brain tumors or infections.
Treatment Options
No Treatment Needed: Some conditions, like anisocoria or Horner’s syndrome, do not require intervention.
Eye Patch: Can help reduce double vision for patients
with third nerve palsy.
Prism Eyeglasses: Special glasses with prism lenses
may relieve diplopia.
Sunglasses: Protect sensitive eyes from bright sunlight.
Eye Drops: Pilocarpine may be prescribed to constrict the pupil in cases of Adie’s tonic pupil.
Surgery: If third nerve palsy persists after six months, surgery may correct eye alignment or drooping eyelids.
Why Choose Bascom Palmer Eye Institute?
Ranked #1 in the Nation
- Bascom Palmer Eye Institute, part of the University of Miami Health System, is the top-rated eye hospital in the U.S., according to U.S. News & World Report.
Patient-Centered Care
- Our team takes the time to understand your unique eye needs, coordinate your care, guide you through treatments, and connect you to valuable resources.
Expert Ophthalmologists
- Receive care from leading specialists using advanced diagnostic tools and personalized treatment plans.
FAQ
What is toxic optic neuropathy, and how does it differ from other vision losses?
What are the main causes and risk factors for toxic optic neuropathy?
How is toxic optic neuropathy diagnosed?
What treatments can reverse or halt toxic optic neuropathy?
How can you prevent toxic optic neuropathy in daily life?
Our Doctors
No doctors available for this speciality.
Questions? We’re here to help.
Our appointment specialists are ready to help you find what you need. Contact us today.
